Understanding Medicaid Fee-for-Service: A Comprehensive Guide
Medicaid, a joint federal and state program, provides healthcare coverage to millions of low-income Americans. Within Medicaid, there are various delivery systems, one of the most prominent being Medicaid Fee-for-Service (FFS). Understanding how Medicaid Fee-for-Service operates is crucial for both healthcare providers and beneficiaries. This article aims to provide a comprehensive overview of Medicaid Fee-for-Service, covering its mechanics, advantages, disadvantages, and recent trends.
What is Medicaid Fee-for-Service?
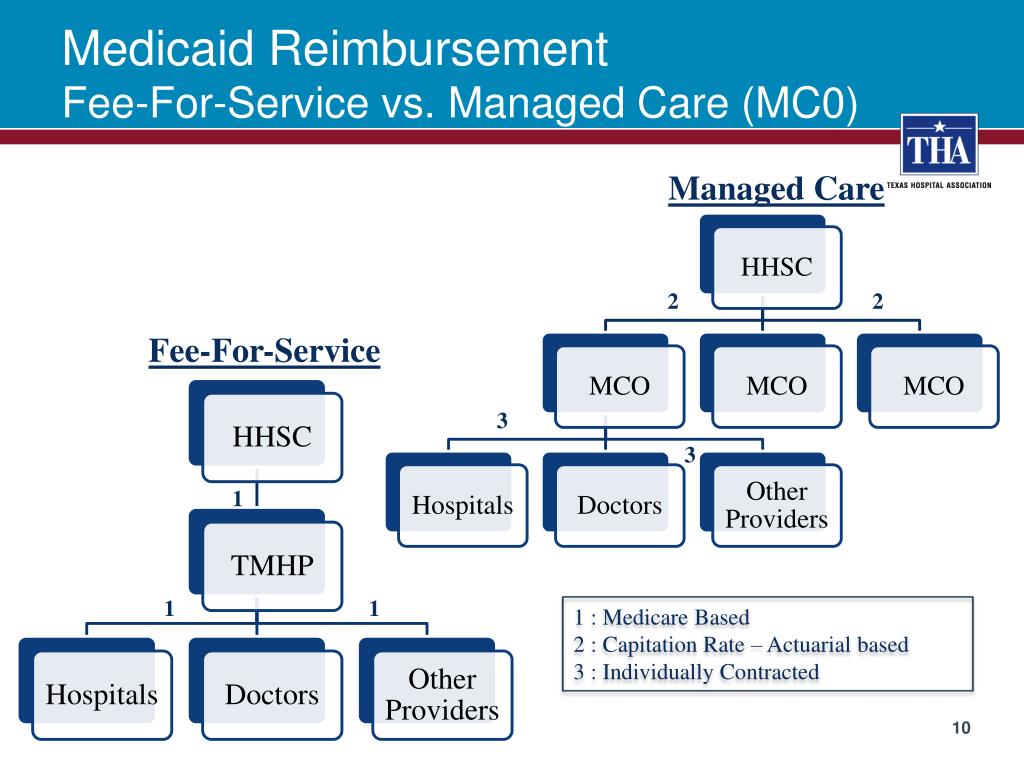
Medicaid Fee-for-Service is a traditional payment model where healthcare providers are paid a fee for each service they render to a Medicaid beneficiary. This is in contrast to managed care organizations (MCOs), where providers receive a capitated payment per member per month, regardless of the number of services provided. In a Medicaid Fee-for-Service system, the state Medicaid agency directly reimburses providers for covered services based on a predetermined fee schedule.
The key characteristic of Medicaid Fee-for-Service is its transactional nature. Each time a beneficiary receives care, the provider submits a claim to the state Medicaid agency, detailing the services provided and the corresponding charges. The agency then reviews the claim and reimburses the provider according to the established fee schedule. This model emphasizes volume, as providers are incentivized to provide more services to generate more revenue.
How Medicaid Fee-for-Service Works
The operation of Medicaid Fee-for-Service involves several key steps:
- Eligibility Determination: Individuals must first be deemed eligible for Medicaid based on their income, household size, and other criteria.
- Service Provision: Eligible beneficiaries receive healthcare services from participating providers.
- Claim Submission: Providers submit claims to the state Medicaid agency for the services rendered. These claims include detailed information such as the patient’s ID, the date of service, the specific services provided (using CPT codes), and the charges.
- Claim Adjudication: The state Medicaid agency reviews the claims to ensure they are accurate, complete, and comply with program rules. This includes verifying the beneficiary’s eligibility, confirming that the services are covered under Medicaid, and checking for duplicate claims.
- Reimbursement: If the claim is approved, the state Medicaid agency reimburses the provider according to the established fee schedule.
The fee schedules used in Medicaid Fee-for-Service are typically determined by the state Medicaid agency and may vary by service type, provider specialty, and geographic location. These fee schedules are often lower than those used by private insurers or Medicare, which can impact provider participation in Medicaid Fee-for-Service programs.
Advantages of Medicaid Fee-for-Service
Medicaid Fee-for-Service offers several potential advantages:
- Provider Choice: Beneficiaries often have greater freedom to choose their healthcare providers compared to managed care models, where they may be limited to a specific network of providers.
- Simplicity: The transactional nature of Medicaid Fee-for-Service can be relatively straightforward for providers who are familiar with billing and coding practices.
- Transparency: The fee schedules are typically public, providing transparency regarding reimbursement rates.
Disadvantages of Medicaid Fee-for-Service
Despite its advantages, Medicaid Fee-for-Service also has significant drawbacks:
- Lack of Care Coordination: The fragmented nature of Medicaid Fee-for-Service can lead to poor care coordination, as there is no single entity responsible for managing a beneficiary’s overall healthcare needs. This can result in duplicated services, unnecessary hospitalizations, and suboptimal health outcomes.
- Incentives for Overutilization: The payment model incentivizes providers to provide more services, potentially leading to overutilization and increased costs.
- Limited Focus on Prevention: Medicaid Fee-for-Service typically focuses on treating acute illnesses rather than preventing them. This can result in higher long-term healthcare costs.
- Administrative Burden: Providers face a significant administrative burden in submitting and tracking claims, which can be time-consuming and costly.
- Lower Reimbursement Rates: Medicaid Fee-for-Service often has lower reimbursement rates than private insurance, which can discourage providers from participating in the program.
Medicaid Managed Care vs. Fee-for-Service
The primary alternative to Medicaid Fee-for-Service is Medicaid managed care. In managed care, states contract with MCOs to provide healthcare services to Medicaid beneficiaries. The MCOs receive a capitated payment per member per month and are responsible for managing the beneficiary’s healthcare needs. [See also: Medicaid Managed Care: An In-Depth Comparison] This model aims to improve care coordination, control costs, and promote preventive care.
While managed care has become increasingly prevalent in Medicaid, Medicaid Fee-for-Service still plays a significant role in many states. Some states use a combination of both models, with certain populations or services covered under Medicaid Fee-for-Service and others covered under managed care. For example, individuals with complex medical needs or those residing in rural areas may be more likely to receive care through Medicaid Fee-for-Service.
Recent Trends in Medicaid Fee-for-Service
Several recent trends are shaping the future of Medicaid Fee-for-Service:
- Value-Based Payment Models: States are increasingly experimenting with value-based payment models in Medicaid Fee-for-Service to incentivize quality and efficiency. These models may include pay-for-performance incentives, bundled payments, and shared savings arrangements.
- Care Coordination Initiatives: Recognizing the importance of care coordination, states are implementing various initiatives to improve care coordination within Medicaid Fee-for-Service. These initiatives may include care management programs, health homes, and accountable care organizations (ACOs).
- Data Analytics and Program Integrity: States are leveraging data analytics to identify fraud, waste, and abuse in Medicaid Fee-for-Service. This can help to ensure that taxpayer dollars are being used effectively and efficiently.
- Telehealth Expansion: The COVID-19 pandemic has accelerated the adoption of telehealth in Medicaid Fee-for-Service. States are expanding coverage for telehealth services and exploring ways to integrate telehealth into the Medicaid delivery system.
Challenges and Opportunities
Medicaid Fee-for-Service faces several challenges, including:
- Controlling Costs: The fee-for-service model can be difficult to control costs due to the incentives for overutilization.
- Improving Quality: Ensuring high-quality care within a fragmented system can be challenging.
- Addressing Health Disparities: Medicaid beneficiaries often face significant health disparities, and Medicaid Fee-for-Service needs to be designed to address these disparities effectively.
However, there are also opportunities to improve Medicaid Fee-for-Service, including:
- Implementing Value-Based Payment Models: Value-based payment models can incentivize quality and efficiency, leading to better health outcomes and lower costs.
- Investing in Care Coordination: Care coordination initiatives can improve the continuity and quality of care for Medicaid beneficiaries.
- Leveraging Technology: Technology can be used to improve care delivery, enhance communication, and streamline administrative processes.
The Future of Medicaid Fee-for-Service
The future of Medicaid Fee-for-Service is likely to involve a continued shift towards value-based payment models, increased emphasis on care coordination, and greater use of technology. States will need to carefully consider the tradeoffs between Medicaid Fee-for-Service and managed care when designing their Medicaid programs. It is crucial to balance the need for cost control with the importance of ensuring access to high-quality care for Medicaid beneficiaries. [See also: Innovations in Medicaid Payment Models] The ongoing evolution of Medicaid Fee-for-Service will play a critical role in shaping the healthcare landscape for millions of Americans.
Conclusion
Medicaid Fee-for-Service remains a significant component of the Medicaid program, providing healthcare coverage to a substantial portion of the low-income population. While it offers certain advantages, such as provider choice, it also faces challenges related to cost control, care coordination, and quality improvement. As states continue to innovate and refine their Medicaid programs, the future of Medicaid Fee-for-Service will depend on its ability to adapt to evolving healthcare needs and policy priorities. Understanding the intricacies of Medicaid Fee-for-Service is essential for policymakers, healthcare providers, and beneficiaries alike.
